The Collaborative Care Model (CoCM) is an evidence-based approach designed to identify and treat behavioral health conditions within primary care settings.
In 2017, the Centers for Medicare and Medicaid Services (CMS) introduced dedicated Current Procedural Terminology (CPT) codes for CoCM, leading many states to incorporate these services into their Medicaid fee schedules.
One of these states is New York, a national leader in supporting the adoption of CoCM statewide. Primary Care IPA (PCIPA) became the first organization in Western New York to integrate CoCM across both adult and pediatric populations, with the latter expansion supported by a SAMHSA-funded initiative.
Despite concerns about financial sustainability, a review of over 12 successful practices across Western New York demonstrates that CoCM can achieve financial viability within months of implementation.
“Collaborative Care is an outstanding example of what we are trying to accomplish in value-based care. It enhances the scope of preventative care provided in primary care settings, minimizes the unnecessary use of specialty care, reduces overall costs, and most importantly, improves care for our patients.”
– Larry Zielinski, CEO, Primary Care IPA

The Financial Case for Collaborative Care
CoCM’s Financial Sustainability: Achieving Stability within Months
| Time Frame | Caseload | Billable Episodes (76%) | Profitability |
|---|---|---|---|
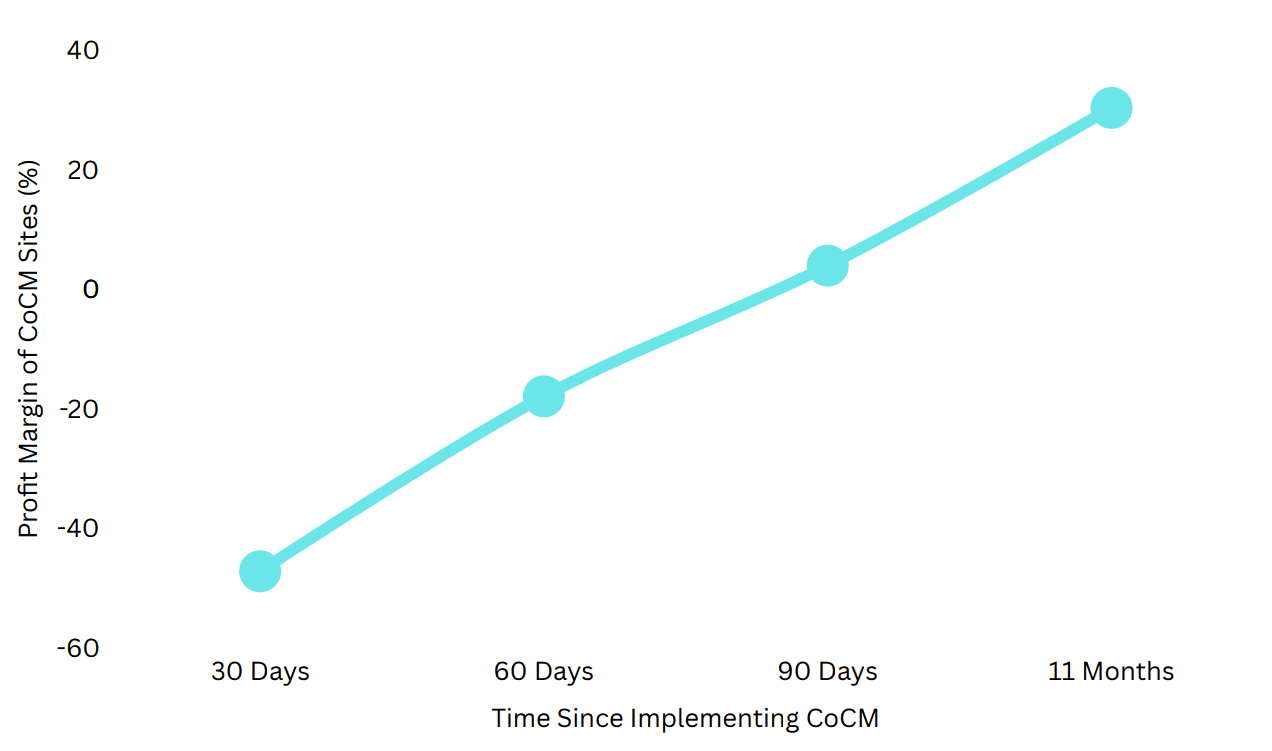
| 30 Days | 51 patients | 39 episodes | –47.2% |
| 60 Days | 65 patients | 49 episodes | –17.9% |
| 90 Days | 75 patients | 57 episodes | +3.98% |
| 11 Months | 80 patients | 61 episodes | +30.4% |
Beyond breaking even, CoCM sites reported a 3.98% profit margin at 90 days. By 11 months, sites reported a 30.4% surplus, proving long-term financial sustainability.
Scalability Across Patient Populations
| Patient Population | Break-Even Point | Avg. Monthly Billing Revenue (90 days) |
|---|---|---|
| Adult | 52 patients | $4,560.01 |
| Pediatric | 53 patients | $4,037.98 |
Clinical Outcomes:
The Case for Integration Compared to National Benchmarks
Quaker Medical Associates: Leading the Way in Clinical Outcomes
- Depression Outcomes (1-Year Data)
- 80% of patients with moderate to severe depression improved within one year:
- 40% achieved full remission
- 40% improved to mild symptoms
- 80% of patients with moderate to severe depression improved within one year:
- Anxiety Outcomes (1-Year Data)
- 60% of patients showed meaningful improvement:
- 40% achieved remission
- 20% improved to mild symptoms
- 60% of patients showed meaningful improvement:
Buffalo Pediatrics: Faster Symptom Reduction than National Benchmarks
- 58% of depression patients improved within 4 months, with 29% achieving remission.
- 57% of anxiety patients improved within 5 months, with 14% achieving remission.
These results not only validate CoCM’s effectiveness in accelerating symptom reduction but also emphasize its broader impact beyond patient outcomes. The following insights from healthcare educators and professionals reinforce how CoCM enhances training for future behavioral health providers, strengthens interdisciplinary collaboration, and equips clinicians with the skills needed to address complex mental health challenges in primary care settings.

“The success of CoCM at Primary Care IPA has given our MSW students real-world experience in evidence-based, interdisciplinary care.”
— Katie McClain-Meeder, Clinical Associate Professor, SUNY Buffalo
Cost Savings and ROI
When fully adopted, CoCM is projected to save Primary Care IPA over $5 million annually by:
- Reducing ER visits and hospitalizations by 25-30%
- Decreasing specialty referrals by 30%, retaining $400 per patient (saving and keeping $32,000+ for 80 patients in-house)
- Boosting medication adherence by 25% and reducing crisis events by 30%
- Billing data confirms CoCM covers staffing costs within 90 days.
By integrating mental health treatment into primary care, CoCM reduces high-cost emergency services, strengthens continuity of care, and ensures sustained cost savings.
Conclusion:
CoCM as the Future of Behavioral Health
CoCM is not just a solution—it is a forward-thinking approach to transforming mental health care in primary care settings.
Authors: Virna Little and Aniece Futch, with special thanks to Primary Care IPA and JG Research & Evaluation

